Resuming uveitis clinical services during the COVID-19 pandemic
Guidance for uveitis specialists for resuming uveitis clinical services during the COVID-19 pandemic
June 23 2020
This guidance addresses factors to consider in resuming services by the Academy of Royal Medical Colleges. We focus on planning for uveitis services during the pandemic outbreak, while social distancing requirements remain and provides resources to help you plan. We are likely to experience a recovery phase where we resume services, followed by a stabilisation phase where COVID-19 restrictions are still present in some form. This period of huge change brings great challenge but also the promise of reshaping our services in preparation for our “new normal", in particular for telemedicine , image transfer and harmonisation. The Service Redesign, Case studies and Technology sections are written with these aims in mind. Guidance for clinical management of patients is here
Contents
- Planning for safety of staff and patients
- Running face-to-face uveitis clinics safely
- Minimising interactions with hospital staff
- Keeping staff safe
- Resuming Service Delivery
- Releasing Capacity
- Triage and Risk Stratification
- Models of care including telemedicine and virtual clinics
- Communications and Shared Care
- Preparing Patients
- Medicolegal considerations
- Quality Assurance / Governance
- Teaching and Training
- Effective Service Design with case studies
- Technology
- Resources
1. Planning for safety of staff and patients
Resuming of ophthalmic services requires consideration of one key priority area of planning: keeping patients and staff safe while a definitive treatment or vaccine against sars-cov2 is found. When you scale-up your uveitis face-to-face (F2F) clinical activity, you will consider waiting room space, physical distancing, time for cleaning equipment, donning and doffing PPE and the patient journey through your department. Inefficiencies in your pre-existing patient pathway combined with these new factors can have a significant impact on throughput of patients and reduce capacity unless they are mitigated.
A robust electronic medical record/paperlite system increases safety, reduces prescribing errors and clinical governance events due to missing data at the point of decision-making. Hospitals may enable development of data collection forms electronically within their Trust EMR or enable upload of data collected on paper to facilitate a paperlite system.
Running face-to-face uveitis clinics safely
- Schedule patients to allow more time, at least until your patient pathway is optimised. E.g 45 minutes scheduling or booking double slots for complex new patients.
- Your hospital may adopt evening or weekend working to ensure delivery of adequate face to face appointments which will allow you to organise clinics safely.
- Your unit may decide to deploy healthcare staff to speed the flow of patients eg marshalls/ runners
- Ask patients to arrive within 15 minutes of their appointment time to avoid waiting.
- Donning and doffing of PPE and of cleaning equipment will take extra time.
- We suggest no more than 5-6 face to face patients per session
- Review patient records and previous imaging prior to clinic
- If helpful, break up new or complex uveitis patient consultations into; a telephone consultation while the patient is off- site, prior to the appointment (e.g the day before) to establish history, problems and review of results. The second visit will be for imaging, examination and a short discussion
- There is early evidence that face coverings can limit virus spread in public spaces. This is not mandatory in hospitals in England but in Scotland but face-coverings are in widespread use in public places.
- Discuss locally how environmental disinfection is taking place and policies for cleaning optos machines or HVF analysers (see manufacturer websites for updates and guidance)
Minimising interactions with hospital staff
-
Think about the patient flow in your clinic and plan the work-force to have the right skills and training to assess your patients and manage them. Non-medical staff may be employed in extended roles, such as in virtual clinics where visual acuities, pressure and imaging can be performed, optimally, by one person to allow a single, time-efficient visit.
- Employ the most effective alternatives to face to-face clinics for your service.
- Telephone or video clinics
- Virtual clinics
- Some units may find shared care with optometry practices local to the patient is the most efficient model for service delivery, especially in remote areas.
- You may find it useful for your AHP ( llied health professional) to speak with pharmacists attached to GP practices to ensure that decisions from telemedicine clinics are carried out or patients are counselled for IMT.
- Keep in mind that another wave of COVID-19 infection may necessitate reduction of routine elective work
Keeping staff safe
- Maintain an adequate supply of appropriate PPE for staff in outpatients, A&E and theatre environments and stay up to date with infection control recommendations.
- Staff-testing is now being widely deployed in many trusts with both antibody and PCR testing for asymptomatic staff members. This will be both reassuring and ensure adequate staffing resource.
- Screen patients for symptoms before appointments or provide patient information by letter about changes to the hospital environment. Patient information is available on www.uveitisstudygroup.org
- Provide access to well- being resources and extra support, especially where there are plans to extend hours of working
- Consider discussing face-coverings when interacting with staff at <2m
2. Resuming Service Delivery
Meeting capacity and predicting the workload of your service is going to take planning. Uveitis services and eye units need to rapidly estimate the maximum capacity they can safely start in the recovery phase. It is likely that your department will have a maximum capacity at any one time so projecting a realistic time for each appointment and understanding the patient journey and other concurrent clinics is vital. Make sure the appointment booking system/staff are involved in new clinic set- up, so that these can be booked properly and that clinical activity is accurately coded.
Telemedicine is divided into synchronous consultations which are in real-time and asynchronous consultations which are aided by store-and-forward technologies. In the latter, data are collected, locally or remotely and forwarded prior to a later date consultation. Health and Social Care Network (HSCN) connectivity replaces N3 connectivity and is now possible between primary and secondary care, allowing information exchange between optometry and ophthalmology services. Remote monitoring is also a part of telemedicine.
Releasing Capacity
Consider discharging patients who are in drug-free remission of uveitis for a long period of time and forgoing follow up patients with known, uncomplicated AAU. It may be appropriate to increase the interval between clinic appointments in those at very low risk of visual loss. For some patients it may be appropriate to offer alternate face-to-face and non-face-to face-clinics. Intermediate uveitis complicated by CMO , inflammatory CNVM, birdshot chorioretinopathy resolving monophasic white-dot syndromes may be suitable a combination of F2F and virtual clnics if not virtual clinics alone. (See Table 2)
Effective triage and risk stratification ( See also UCSG clinical guidance)
We suggest uveitis service to triage patients or risk-stratify and allocate patient care according to “right time, right person, right place”. This enables appointment allocation by urgency, the most appropriate consultation modality (Table 1) and the most suitable personnel. See RCOphth guidance on prioritising appointments here.
Effective triage helps to quantify the demand for future outpatient appointments within the models of care you feel work for your service. The capacity/demand modelling can then be planned for the uveitis service.(Table1) Additional clinics may be required with longer work days or weekend-working to meet patient demand. Your job plan is likely to change to reflect your new service model.
Table 1 Case Prioritisation
To be updated soon.Thanks for your patience
This is a suggested follow-up frequency plan for adults patients depending on phase of disease activity.
Table 2 Guide to allocation appointment modality*
|
Telephone/Video (e.g by an AHP/ shared care with an optometrist |
F2F/Virtual alternating appointment** |
F2F** |
|
Anterior uveitis (normal IOP) |
Inflammatory CNV |
1st attendance/ vulnerable adults/ one eye |
|
Scleritis follow up |
Multifocal choroiditis / PIC |
Endophthalmitis |
|
Episcleritis |
Peripheral vasculitis |
Active panuveitis |
|
Counselling for IMT |
Ocular cicatricial pemphigoid |
Corneal inflammatory disease |
|
Prepare history prior to day of clinic |
Toxoplasmosis |
Vasculitis at the posterior pole |
|
|
Anterior/Intermediate Uveitis with cystoid macular oedema |
Active uveitis with secondary ocular hypertension/ glaucoma*** |
|
|
Post intravitreal implant*** |
Asymptomatic uveitis eg JIA |
|
|
Quiescent panuveitis, IU, posterior uveitis |
Unexplained reduced vision/ high risk of visual loss in follow up |
*This is a suggested guide, your case allocation may vary based on your clinical judgement
**New patients could be seen F2F but could be followed with alternate virtual/ F2F virtually or in some cases, just virtual follow up may be suitable according to your judgement. Suggested standard virtual clinic dataset: VA, IOP, Optos, CMO+ AF for choroidal disease
*** IOP may be measured in the community and data shared with your service to reduce frequency of hospital visits
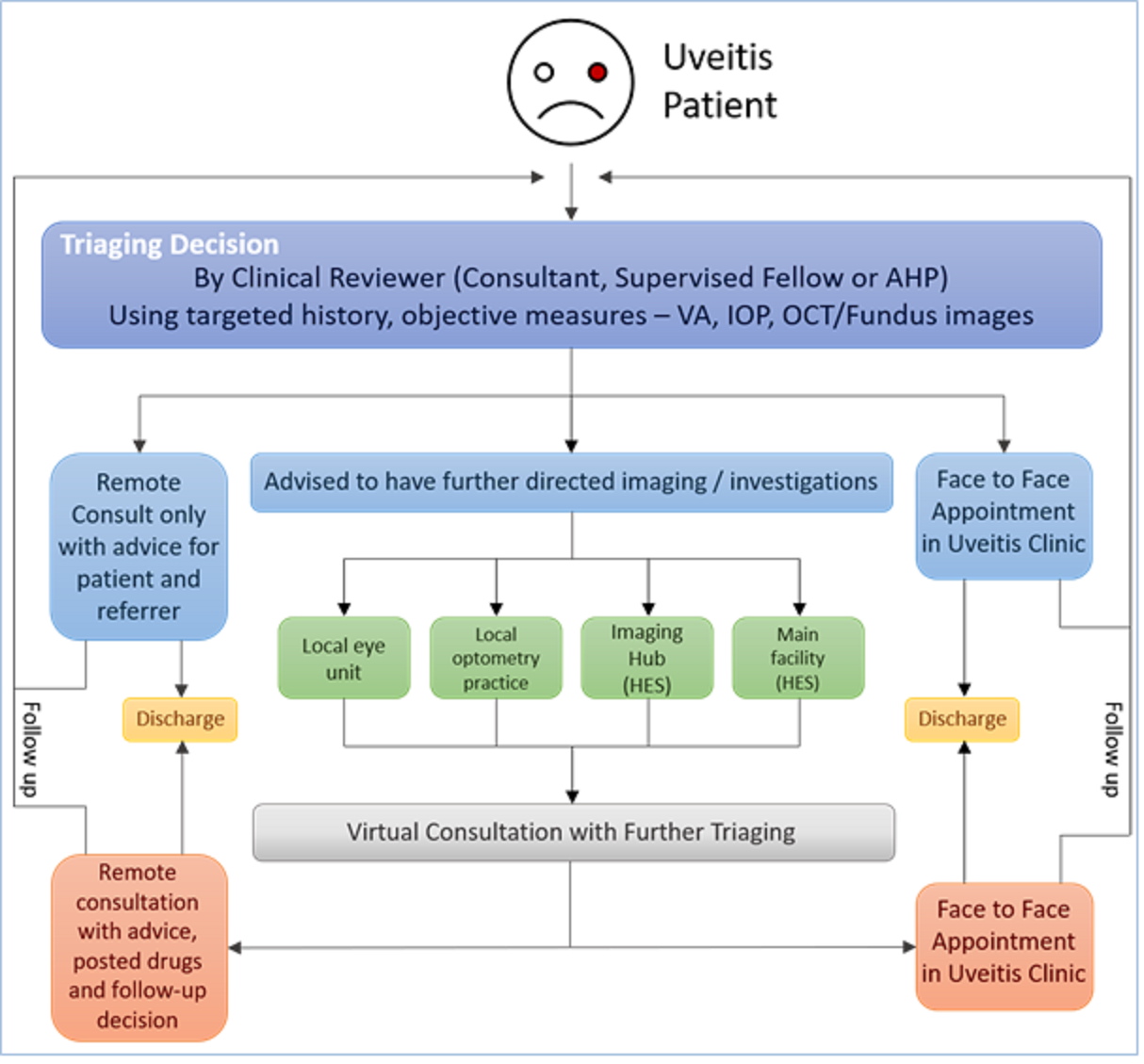
Models of care (Figure 1)
1. Adapt your existing clinic models to take into account measures to reduce patient journey times in your clinic, physical distancing in clinic, time for donning/doffing of PPE and cleaning of equipment factored into clinic capacity.
2.The COVID pandemic has increased the uptake of remote consultations by telephone or video to the ophthalmology care pathway by acceleration of a national pilot using Attend Anywhere videoconsultation service with local information governance approvals in place by April 2020. SeeRCophth webinar on video-consultations on future NHS uk website ( registration required)
- Add a virtual (store and forward) arm to your service, whether the imaging is performed locally or remotely for cystoid macular oedema or mainly retinal/choroidal disease. These are followed by a telephone/ video consultation.
3. The link with primary eye care in optometry has strengthened with two models of linked care possible (The Service Design and Technology sections will expand on this)
- Optometry practices acting as ‘virtual' clinic hubs collecting objective data on uveitis patients such as VA, IOP and in the future OCT/Fundus images. Then transmitting this data directly to hospital eye services (HES).
- Shared care pathways with linked medical records, imaging databases and prescribing rights that could allowed suitably trained and accredited optometrists to co-manage ‘simple' uveitis with HES or IOP monitoring.
Figure 1. Service Delivery Models in Uveitis
This overview of service delivery models in uveitis starts from the point of triage. Not all delivery types will be suitable all services, and some will take time to establish. Select the ones that are right for you and plan the numbers of patients who may be seen by each route to judge capacity for your service. See Service Design to help you plan.
3. Communications and Shared Care
Communication with other professionals
We can apply common principles for robust communication to manage shared care referral pathway in order to minimise travel and hospital visits for patients. ( See Technology) Below are resources and guidance for optimising shared care pathways.
- Agree referral protocols with your local network of referring consultants. Offer a protocol for relevant tests/investigations based on presentation.
- Share test results using a nhs.net email for your service as a starting point for use by the referring network of doctors, GPs, patients and pharmacists. Keep data linked to the hospital record.
- Image sharing If your network uses a PACS system, share images in both directions between referrer and specialist unit, as we do for radiology images eg E2E transfer of OCT on Heidelberg machines. If not, share electronically and save the images in the patient's records in both units. Access to original images will aid diagnosis, minimise hospital interactions and duplication of effort, and may enable the uveitis clinic appointment to be virtual.
- Shared Care Protocols for GPs are important in reducing patients' travel to hospital for routine blood monitoring and maintaining uninterrupted medication supply especially if a GP also has access to a secure email address to share results. These protocols are developed in partnership with secondary care and may posted publicly and shared with the GP at the point of prescribing.
Blood monitoring intervals may be extended to 3 monthly to 6 monthly in patients who are stable on immunosuppressive medication. Summary of COVID-19 medicines guidance: Musculo-skeletal specialist Pharmacy Service. Phlebotomy services in primary and secondary care should provide booked appointments which maintain social distancing.
- Shared care with local optometric practices for example for IOP checks or OCTs to monitor response of CMO to treatment, would reduce travel and need to attend clinics, but usually require service contracts .
- Information exchange between primary and secondary care providers is now ‘live' in some areas. Some of the data held in GP practice EMIS records are available to hospital specialists. Find out if this is active in your area by contacting your CCG or CIO ( chief information officer).
4. Preparing Patients
We are adopting new service delivery models at an unprecedented rate of change. Patients may require reassurance on local measures for their protection and safety, particularly regarding social-distancing, use of PPE, avoidance of prolonged waiting and new ways of working to minimise close contact with staff and other patients.
Keep patients up to date on how new models of service delivery will affect them and your response if further lockdowns happen in your area. If telemedicine or virtual clinics are new in your service, communicate how safety and quality of care are maintained including greater consultant involvement in decision-making and supervision of care.(See UCSG Resources)
Information should be accessible to all patients and parents/guardians with adaptations non-English speaking patients and visually impaired patients, including large print and audio descriptions. Your media and communications team may help with this.
Suggested routes of communication about services:
- Written leaflets/patient information documents in large print. ( Some patients do not have internet access)
- Use your Trust website to update patients. We suggest information includes videos/photos of clinical settings showing social-distancing and staff using PPE. Here is a video which you can use.
- Distribution via local/national eye charities, visual support groups
- Patient webinars (local and national. Signpost patients to www.uveitisstudygroup for national webinar details)
- Direct patients easily and automatically to online patient information in signatures within emailed correspondence.
- Communications can also be sent to your media department about your service and distributed via social media.
5. Medicolegal Considerations
NHS trusts have increased their indemnity through NHS Resolutions to include COVID-19 related practice. From our correspondence with NHS legal teams, NHS doctors will be indemnified during the pandemic including work in roles for which they are not principally trained eg running a COVID-19 ward. If in doubt, contact your legal team.
Generally it is considered that there is implicit consent when participating in a video-consultation. We've summarised good practice for video and telephone consultations below.
- Work in a private place without interruptions
- Check your patient's identity
- Have relevant information about your patient available eg imaging, test results
- Make sure the limitations of the video consultation are made clear and triage to a face to face consultation if your assessment of risk changes as a result of this consultation.
- When discussing procedures/ new medication ensure you document discussion of the procedure, indication and alternatives including no action, risks and benefits.
- Provide login information about video consultations in advance
- Document information shared especially discussion of medications and procedures .
- Check your patient's understanding of the discussion if relevant.
- Correspond with GPs and patients as for a face to face consultation.
Additional resources:
- GMC Guidance (https://www.gmc-uk.org/ethical-guidance/ethical-hub/remote-consultations).
- MDU (https://www.themdu.com/coronavirus
- MPS (https://www.medicalprotection.org/uk/articles/webinar-recording-remote-consulting-during-the-covid-19-outbreak)
- MDDUS (https://www.mddus.com/advice-and-support/advice-library/coronavirus--covid-19) have important information and useful resources on new ways of working, medico-legal issues around remote consultations, as well as working in unfamiliar settings.
6. Quality Assurance/ Governance
The degree of change in uveitis practice requires us to collect data about the way in which services are running and any adverse clinical outcomes that may have occurred during the pandemic. Guidance about clinical audit may be found on RCOphth COVID-19 resource page. The below guidance is aimed to increase the quality of our interactions with patients but also to capture outcomes during this period.
- Use an electronic medical record / go ‘paperlight' wherever possible.
- Maintain patient confidentiality despite relaxation in some information governance
- Use video- consultation platforms approved by your Trust
- Ensure patients whose appointments are postponed/cancelled during the pandemic are identifiable based on your local appointment booking system to avoid loss to follow up.
- Relax DNA (did not attend) discharge policies to allow patients who DNA uveitis clinic appointments during the pandemic further opportunities for review.
- Check that patients received communication containing recommendations for shielding.
- Use e-prescribing on your hospital's electronic medical record or seek the assistance of your pharmacy team. If neither are available/suitable, communicate electronically with the patient's GP practice to ensure timely prescriptions.
- Provide contact information for your eye casualty and/or uveitis department, (see ‘Preparing your patients' section
- Plan service evaluation/ clinical audit, and research projects to develop the evidence base for new ways of working/new protocols/new clinics using RCOphth/ USG guidance as benchmark standards during the pandemic
- Consider recording prescribing changes using pharmacy or electronic prescribing datasets.
- Prospectively collect datix events/ adverse outcomes for uveitis patients in collaboration with your local governance team, including adverse outcomes which may be attributed to DNAs to hospital during the pandemic.
- Encourage participation in patient and staff surveys to assess acceptability of new ways of working. (There is currently a national telemedicine survey study taking place)
7. Teaching: Keep calm and Telecon!
There are fewer opportunities for face-to-face (F2F) assessments of patients in the current climate. Fortunately, uveitis provides excellent subject matter for virtual teaching as much of our decision making is based on laboratory results, retinal imaging and functional measures. Time on a surgical simulator will help maintain surgical skills.
Virtual teaching - Opportunities:
- Greater flexibility – trainees can attend all or some
- There is a huge array of remote learning opportunities nationally and internationally via webinars
- Teaching can be accessed from home or on the move and has the added benefit of keeping those who have to work from home connected with the team.
- Teaching can be more easily recorded and shared eg on deanery websites
- Plan a variety of ways to teach. A pre-clinic discussion of cases and planning or post clinic MDT can all be done virtually and provide trainees with useful guidance directly related to their clinic duties. Message trainees a case of the day/week – this can trigger discussion to reach diagnoses and fosters team-working.
- It's surprisingly feel-good: trainees really appreciate it
- Maintain surgical skills by formally booking sessions on a surgical simulator using a deanery-wide rota.
Virtual teaching – Suggestions for a good teaching session
- Start and finish on-time
- Having a moderator helps run the session well.
- Patient confidentiality is a serious consideration especially when sharing information can be recorded and widely disseminated. De-identify all cases and use hospital-approved video-conferencing software wherever possible.
- Keep a ‘virtual waiting room' if discussing cases.
- Use case examples to simulate experiental learning in clinic sessions
- Encourage participants to ask questions or put their hand up virtually. Frequently stop to ask for any questions/comments to trigger discussion, rather than leaving to the end of the session.
- Collect feedback and adapt your style and content.
- Background noise – ask people to mute unless speaking. The moderator can unmute
- Ask people to interrupt via chat so the moderator can see
- Trouble shoot and do a test-run before your first session as firewalls and IT department management of software can limit accessibility.
8. Service Redesign
Improving your service with telemedicine or departmental re-design, can be made much easier and more effective by tapping into resources and reviewing successful case studies. NHSE have set up the Future NHS collaboration platform which is full of resources and tried and tested guidance for Ophthalmology redesign. We will add case studies for uveitis at the bottom of this section by your colleagues as they come in.
a. Step 1: Start with great resources by registering for an account on Future NHS collaboration platform. Select 'elective care community of practice', then Ophthalmology and RCOphth resources.
b. Keep patients central in your plan. The NHSE/I Eyes Wise program collected the opinions of >100 patients about their services. Case studies for improving patient experience.
c. Who are your stakeholders? Plan for partnership, asking about the agendas and goals of each group. This alignment will give you a much better chance of success. Your stakeholders may include,MECS, LOCSU, service administration/operations manager, IT, imaging lead, patients, commissioners and your regional STP team. Going down a regional (STP) collaborative route might be the best plan if your commissioners want to develop regional provision.
d. Who will help you? Clinical Lead/ director, divisional directors, transformation team, digital innovation team, finance team, improvements team, business planning team.
e. Find out if there is a published regional plan for Ophthalmology outpatients transformation.
f. Share your ideas for good practice using this NHSE easy- to-fill- in template (See Uveitis CSG Resources) and email info@uveitisstudygroup.org
Case studies
o Iain Livingstone, NHS Scotland. There is a national program for remote videoconsultation with direct streaming of videoconsults between Optometry and Secondary care. Follow the links in this document to view NHS Scotland's vision for ophthalmology in communities and find out how and what kit you need.
o N Capewell, A Denniston. Moving secondary care out to the community "At University Hospitals Birmingham NHSFT, we are partnering with one company with a few local optometrists to trial specialist telemedicine software ( Big Picture Medical) that can securely transfer test results, such as eye scans and visual field tests, from their practices to the hospital. Doctors are then able to quickly review the results, decide on a course of action and feedback to the patient via email, without them needing to attend a separate appointment. The hope is that this will make these services more accessible to patients requiring frequent monitoring, whilst reducing the number of visits to the hospital."
o F Quhill IOP measurement for uveitis patients. Currently a few patients are able to have IOPs checked in the community as agreed on a case by case basis with some optometrists in Sheffield. A remote monitoring pathway is being negotiated with the local optometric network ( PEARS) and the Trust.
9. Technology and Systems
A brief guide and a multiple links to technologies available follows. The benefits are rapid access to specialist opinions, convenience for the patient and time saving for the referrer and specialist. There are three key applications of these technologies in uveitis.1. Virtual Clinics using store and forward technologies, interfacing with our EMR for a whole system approach 2. Live consultation between primary care and secondary care 2. Counselling, discussion with patients and some evaluation 3. Live regional uveitis network case referral and shared care by streaming live uveitis specialist consultations between patients, referrer and uveitis specialist and other specialists eg rheumatology.
- The telephone- effective, quick, and ubiquitous
- Home testing: Visual acuity with i-Sight test pro or Peek acuity & monitor distortion using RAMMA
- Telemedicine Video consultations using Attend Anywhere or AccuRx (Specssavers are using this for their patient to optom remote consultations )
- Telemedicine Plus. Video consultation software linked to video-slitlamps or a slit-lamp mounted ipad. Click here for further help and kit. This can connect primary to secondary care in real time or between secondary care e.g for uveitis regional networks.
- Image transfer via store and forward technologies. Image transfer from outside your hospital into your hospital will usually need HSCN connectivity at both sites.
o Camera elsewhere direct into your local server / PACS system: e.g OPERAS
o Camera elsewhere to your system via API or proprietary portal through cloud sharing of images eg.g Big Picture Medical
o vCreate
- Whole system approach:
o Store and Forward using documentation and image sharing using Open Eyes portal in primary care to Open Eyes Ophthalmology EMR in hospitals
o Store and Forward using documentation and image transfer from virtual clinic monitoring via cloud sharing using e.g Big Picture Medical.
- Whatsapp style communication but with IG approval between Optometrists and Ophthalmologists and between Ophthalmologists eg. PANDO, Hospify
- Patient Knows Best Designed for patients who want acces to their records all in one place and more control over their healthcare decisions.
- Electronic Medical Record. There are obvious advantages to Ophthalmology-specific structured datasets or auditable data-fields such as those in Medisoft and Open Eyes. Although, Open Eyes has a uveitis module, no EMR has deployed a structured uveitis dataset. This is necessary to promote uniform clinical data collection and facilitate clinical research on a larger scale. However, the Open Eyes does enable development/improvement of modules with clinician collaboration.
10. Resources
-
RCOphth Recovery Guidance https://www.rcophth.ac.uk/wp-content/uploads/2020/04/Reopening-and-redeveloping-ophthalmology-services-during-Covid-recovery-Interim-guidance-1.pdf
-
Summary of COVID-19 medicines guidance: Musculo-skeletal specialist Pharmacy Service
-
GMC Guidance (https://www.gmc-uk.org/ethical-guidance/ethical-hub/remote-consultations)
-
RCOphth document on digital technology and telemedicine platforms
Service Redesign Resources on NHS Future Collaboration Network ( You'll need to register to access these)
- Webinars for redesign in Ophthalmology
- Ophthalmology redesign handbook including sections on virtual clinics
- NHSE case studies for successful service redesign
- Get It Right First Time (GIRFT) is an initiative which specifies standards and areas for improvement in several areas within Ophthalmology